Goodness. It’s been a while between blog updates. Where has the time gone?! Writing up the case studies is proving incredibly time consuming, and getting the structure and content ‘just right’ is a uniquely challenging process that is often uncomfortable and a bit messy. We know that great things never come from comfort zones, so it’s looking like my thesis is going to be amazing!
Doing a PhD is different to what I imagined it would be. It’s difficult to work out what formulas to follow, and feels impossible to get thing right the first time. Sometimes I just don’t know where to turn to get the answers I’m looking for. And sometimes I don’t realise that I’ve found the answers already, because they’re not what I thought I was looking for – which makes them difficult to recognise until much later than I’ve found them. Eventually I seem to always get there. But it’s not until I’ve waded through the ocean of support, advice and recommendations which comes my way, trying to catch onto the most important clues, hints and tips to get me on the right path. I’ve dusted myself off from so many trips and stumbles on this journey, and I’m constantly learning along the way.
Reminds me of being a new parent, and particularly a first-time mum. The learning process never ends, and it’s difficult to feel like you’ve got things just right. And even when you do, it’s usually short-lived because your child has grown, things have changed, and you need to adapt how you’re managing to make the engine’s run smoothly again and navigate to recover coordinates for the course you’re on. And then repeat.
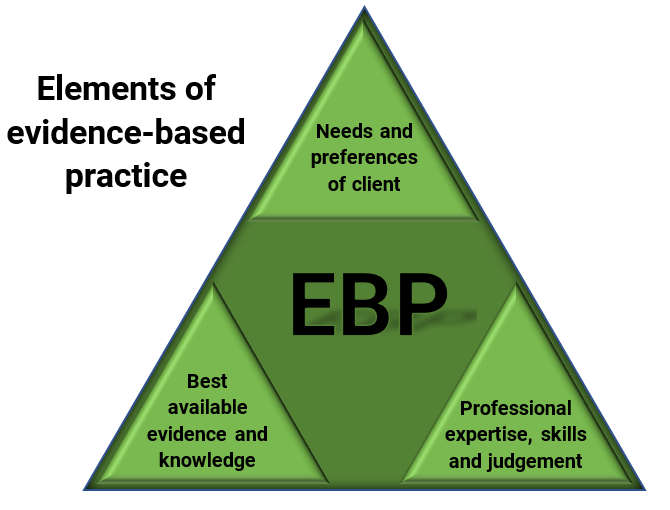
So how can we support new mum’s through this process? What evidence can we draw on to inform practices and feel confident that the advice and recommendations we’re making constitute EBP?
Occupational therapists pride themselves in offering person-centred practice. Reminding ourselves of the EBP triad is critical when we’re reflecting about our practice, and touching base with benchmarks underpinning our professional integrity. When we’re searching for the best available evidence and knowledge in literature, we need to remember this is just one element of EBP. Sometimes the information we find might not match the issues, needs or circumstances of the person whose goals we’re supporting. Do the needs and preferences of any client trump the literature? Is it ‘EBP’ if we offer practices that are not strongly backed by literature because in our professional experience they seem to work?
Reflecting on my clinical practice experiences, the case studies and talking with my colleagues and supervision team, I can’t help but consider that so many OT’s feel a sense of awkwardness and discomfort when they offer interventions and assessments that are not in keeping with recommendations in the latest literature. I know I often do. But more recently I’m starting to realise that EBP is about achieving balance between the three elements in the triad. There’s an art form in tailoring dynamically balanced services to meet a person’s needs to the best of your professional ability – and within professional scope of practice.
Our client’s employ and engage with us to achieve goals that they have chosen, want or need. And most of the time they’re pretty clear about what those goals look like. It’s up to us to make it work. For them.
So many of the OT’s told me in the case studies that the only outcome which matters in EBP is the client achieving a goal in the way that is meaningful and satisfactory to them. It’s easy to see this is person-centred practice. Is it EBP? Yes, I think most definitely so.
More questions? These articles might offer more food for thought:
Lampe, A., Mu, K., Qi, Y., Wang, Y., Brown-King, K., Moran, B., & Talian, E. (2019). Evidenced-Based Practice (EBP) as Perceived by OTs and PTs. American Journal of Occupational Therapy, 73 (4_Supplement_1) Click here to access
Myers, C., DeMaria, S., & Pomeranz, J. (2019). The Development of Evidence-Based Practice (EBP) Competencies in OT: A Modified Delphi Study. American Journal of Occupational Therapy, 73 (4_Supplement_1). Click here to access