This Photo by Unknown Author is licensed under CC BY-SA
I’ve been thinking for a long time that someone should develop a model for co-occupations. There are times that we need to improve how we understand, address and nurture the mother-child dyad through shared occupational intentionality and engagement during all daily life routines, in the context of both maternal and child development. There’s a lot that can be addressed in the name of co-occupation.
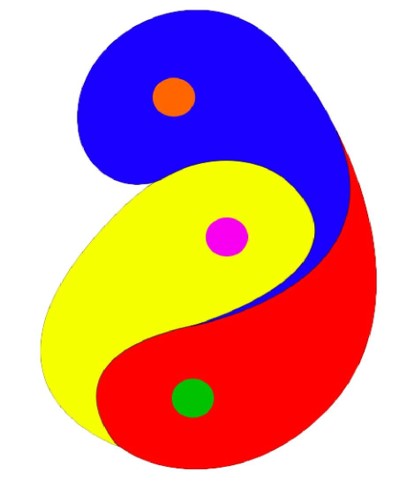
I’ve just stumbled across this image in a creative commons by an unknown author. I wish I knew who made this graphic so I could learn about why they made it and what it means to them. But for me; This is it. This visually conveys the heart of co-occupation and the inseparability of mother-infant dyad. I like that it also reminds us that the mother-infant dyad is not separate from others. Co-parents, partners, other children… whoever is at the heart of the ‘person’ in person-centered care.
It also represents that a person’s sense of self and life meaning expands and shifts when they become a parent, as mothers might experience during matrescence, and fathers during patrescence. We begin to think of others more in our occupational engagement, and the meaning for them with actions and participation becomes part of the meaning for us.
On a side note, I did start to wonder about which co-occupations which OT’s would address as part of women’s health during motherhood stages. Is sex a co-occupation? I think it might be. The OT textbooks are usually all about sex in the context of a person managing issues due to disability and physical dysfunction, but I did recently stumble across an person-centered OT model titled, “The Occupational Therapy Sexual Assessment Framework” (Walker, et al, 2020, p. 5), which seemed a bit more flexible. So interesting. I’m not sure that this is part of this PhD, but I do think there’s grounds to consider this at some point. Later. Maybe.
It’s easy to get the impression that co-occupations are difficult to understand and challenging to integrate into practice in a meaningful way. There are many OT’s who have adapted co-occupations into their practice, but many more haven’t. Without knowing how to contextualise the place and value of co-occupations in person-centered care, it’s difficult. Doidge (2012) completed and published a PhD thesis is available on co-occupations in motherhood, which is brilliant. There’s a link to it in my “Library“. There’s also Esdaile and Olsen’s (2004) textbook about mothering occupations, which talks frequently about co-occupations. The more we use words like co-occupations and matrescence, the more they start to become part of our vernacular, which changes the way we conceptualise and practice. We’re on the way, aren’t we?
I’m so close to being finished my thesis now, and I can’t wait to share the findings. I am so grateful to the OT and consumer participants who shared their experiences, thoughts and perspectives for the PhD. And to the patient and generous people who have talked with me since to help me make sense of what it all means. I can’t wait to share my research. I truly hope others can enjoy learning how amazing these OT’s are in their roles supporting women address health issues and wellbeing needs throughout perinatal stages and matrescence as much as I have.
References:
Doidge, K. (2012). Co-occupation categories tested in the mothering context. (Master of Occupational Therapy), Otago Polytechnic, Dunedin, New Zealand.
Esdaile, S. A., & Olsen, J. A. (Eds.). (2004). Mothering occupations: Challenge, agency and participation. Philadelphia, USA: F. A. Davis Company.
Walker, B., Otte, K., LeMond, K., Hess, P., Kaizer, K., Faulkner, T., & Christy, D. (2020). Development of the Occupational Performance Inventory of Sexuality and Intimacy (OPISI): Phase One. The Open Journal of Occupational Therapy, 8(2), 1-18. https://doi.org/10.15453/2168-6408.1694