As OT’s in non-traditional areas of practice, I think there is often a struggle with imposter syndrome and that haunting reputation of ambiguity in professional practice. We doubt ourselves so often, wondering if our practices are within scope, and feeling a little blurry about how they relate back to occupation. I’ve been a bit unclear recently about a few concepts as I’m coding the case study transcripts, and have been reflecting on how well do I feel I understand OT roots. I was surprised to find I didn’t feel as confident as I thought I should have. So, I’ve been going back to basics. I’ve gone to the annexes of the library and dug out a handful of texts that I felt I needed to brush up on.
The book which has struck me most today is about occupational science.
Zemke, R., & Clark, F. (1996). Occupational science : The evolving discipline. Philadelphia: F.A. Davis.
When I attended and presented about my research at the COTEC-ENOTHE Congress in Ireland a few years ago, I was surprised about my research being categorised under ‘occupational science’. I received some significant feedback during that session from some leading European OT’s and who were very well versed in occupational science, which I found really challenging at the time. They recommended strongly to me that I should familiarise myself with occupational science as a priority. I must confess it’s been on the backburner a bit since then, but I’ve just reached a point with my research now that the knowledge gap is starting to impact on the quality of my work.
As an OT, I often struggle to accept the relevance of occupational science to OT practice. I wonder if this is similar for OT’s practicing in other parts of the world? I’ve been reading this primary occupational science text, and keeping my mind as open as possible. I’ve decided to embrace the challenge, and really learn about how we fit together, and why occupational science is so relevant to perinatal OT practice.
Did you know one of the primary reasons occupational science exists is to help the OT profession grow and evolve into the 21st Century? Until a few months ago, I didn’t.
Part of the reason occupational science was developed was to offer a “framework for understanding the relationship of biology to meaning”, and that “if occupational science and occupational therapy are truly integrated, new clinical approaches may emerge that … suggest some new or expanded directions for practice”, which “can be used to improve patient care” (Zemke & Clarke, 1996, p. 325). What more could we ask for?!
The clues about the relevance and pertinence of occupational science for perinatal maternal health have rolled out in droves as I’ve read many chapters, but especially in these sections:
- Section V: Co-occupations of mothers and children, pp. 213-216.
- Chapter 21: Games mothers play with their full-term and pre-term infants, pp. 217-226.
- Chapter 23: A Phenomenology of motherhood, pp. 243-246.
I have quickly found many favourite quotes from this textbook, but I think today this one is striking a chord:
“There are two kinds of visionaries: those who go after the holy grail without caring who they stomp on in the process because their eye is on some specific future goal, and those I call peripheral visionaries who work on the tasks of today and tomorrow with their eyes open, with a breadth of attention and vision that is inclusive and holistic. Occupational scientists and occupational therapists are called to be the second kind of visionaries, to bring the breadth of their attention and an inclusive holistic vision to bear on occupation in human life and in health” (Zemke & Clark, 1996, p12).
An old friend and I caught up a little while ago, and she asked me if I’d ever heard of anyone having any strange and unexpected neurological symptoms after the “normal” and “uncomplicated” birth of their child. I shared a little about what I head learned in my research studies, and asked her why she was interested. With tears in her eyes, she told me that her last child’s birth had “ruined her”. Suddenly I noticed the way she was walking – her gait pattern was ataxic and she was managing minor foot drop. Her upper limb control was also obviously impacted. If I had not have known differently, I would have assumed she was presenting with minor stroke symptoms. Aside from this, she was just so clearly personally and emotionally affected by this issue, as a person and as a mother. We had a conversation about what had happened to her during and after the birth, and her struggle to find a medical practitioner or specialist who could offer a diagnosis and treatment plan. She is a highly competent and capable person with strong medical literacy, and in after a year of searching is still no closer to finding any answers. Right now, her life seems forever changed, and my heart broke a little seeing the emotional toll it was having on her.
I have searched a little for clues in the literature about this kind of issue, and was able to quickly find three articles which discussed awareness of this issue, but there was very nothing to be easily found about who can help women rehabilitate and recover their functional capacities following such events.
I know this search is only scratched the surface of this issue, but it made me think about the impact on my friend. Her sense of isolation, disempowerment and helplessness with being unable to diagnose and address her issues was unforgettable. I wonder how many other women are out there feeling like my friend does? It’s now on the list of things that need to be included with this PhD, and I hope that there may be some answers on offer and accessible help available in the near future for anyone suffering in this way.
I’m still coding interviews in the case study, and am distracted by ‘what if’s’. As I pull apart what this sample of perinatal OT’s are doing to support women, I’m wondering more and more about how different my two motherhood experiences might have been, if I’d been able to access any one of these perinatal OT’s.
Today I was thinking about my cultural beliefs and unique life choices – which are as unique to me as they are to every single person. We are all so different. I was reflecting on how amazing it would be to have access a maternal health OT who had the professional scope and capacity to understand my personal goals and issues, then tailor a huge range of services to support my unique needs, AND be available at any perinatal stage. Wowsers. Yes, please.
Each OT is in their role for a different reason and purpose, and the practices and outcomes are remarkable in their scope, variety and degree. And this is only the beginning. Keep it up, perinatal OT’s!

A colleague and I were laughing this morning about her daughter’s idea of “Womb in a Room”. Her daughter sees herself having children in future, but has no desire to ever be pregnant – it interrupts your career, your lifestyle, you relationships and social life, your bodily functions and capacities, and a whole heap of other things. It’s inconvenient. So she had the idea of “Womb in a Room” – where you could have an external womb in the room: You can watch your baby grow, and get on with your life in the interim. I remembered seeing this YouTube video years ago about the incubator pod – it’s exactly a “Womb in a Room”. We laughed as we watched the YouTube clip, but by the end of it we were both feeling quite sober.
So many stages of perinatal transitions interrupt women’s routines, schedules and functional performance capacities. It’s a big deal for many women. This clip made me consider that there are many ways to tackle this issue of inconvenience. One way is, conceptually, to outsource your pregnancy to incubation pod. I’m a sci-fi dork through and through. I love it, and I’m excited by the futuristic fantasy of this on a conceptual level. But sitting here in real life, I’m finding myself deeply confronted by this piece of technology, and have decided I’m not really into the pod. Whilst I think this might conceptually be an incredible technological innovation for helping premature babies to safely develop in a controlled environment outside of the natural womb; for me, the buck pretty much stops there.
The ‘inconveniences’ of perinatal transitions are real, and they truly do need to be addressed. Women need to feel they are empowered to choose whatever lifestyle they like throughout motherhood. I hope that the future will be full of OT’s supporting women throughout perinatal stages, so they can lead their very best lives as women and mothers. And a few pods to help families in special circumstances, and for premmie babies have the best shot they can. Who knows what the future will hold? But what an amazing world we live in ♥

I got a little bit over the coding and thematic analysis today, so played with making a wordblob while I was procrastinating. I love this, and it made me have a little giggle. “Yeah”, is what I kept repeating throughout these interviews. Listening to OT’s describe their role in perinatal health was something I just totally understood, and often there wasn’t anything else to say. Yeah”, I get it. It was a complete joy to interview these OT’s, and it’s changed the way I look at my profession, and perinatal populations. I am looking so forward to finally being in a position where I can publicly present these findings.
A colleague just forwarded me this article from the Guardian, titled:
… and it got me thinking…
- OT’s work with clients to address needs relating to driving and car transitions/access and adaptations/modifications
- OT’s work with women during all perinatal stages
- OT’s are specialists in ergonomics for maximising safety and capacity with occupational function
- OT’s work with adaptive aids and devices
… have any OT’s come up with solution to this issue yet?
Today’s new word:
“Matrescence”: The birth of a mother
Originally coined in 1975 by an American medical anthropologist named Dana Raphael, this word feels like the missing link I’ve been looking for with my research this month.
Dr Aurélie Athan and Dr Alexandra Sacks are two of many people devoted to reviving the term, and I can’t wait to explore how relevant is it to perinatal occupational therapy. Very exciting times!
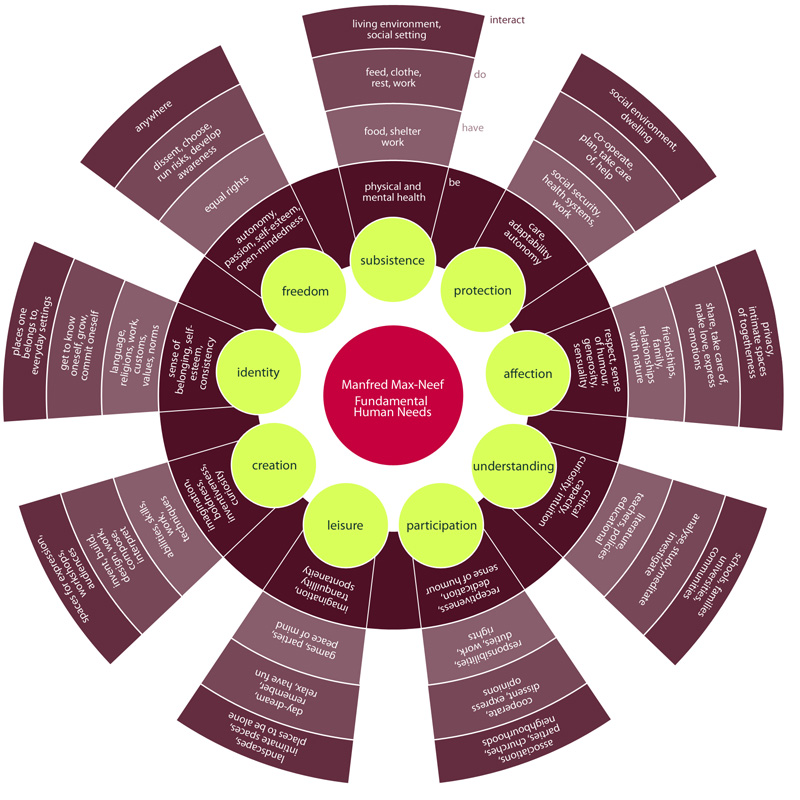
I’ve been thinking a lot about what women need during perinatal transitions, and today I’ve come across a model of fundamental human needs by Max-Neef (1986) that I had never heard of before. Looking at it – as an occupational therapist – I’m excited. I can see here a model which looks at individuals through a similar lens to occupational therapy. It’s complex, and I’m just starting to explore how relevant it might be to my research, but I’m so curious to see where it may lead…
Wheel of Fundamental Human Needs (Max-Neef, 1986)
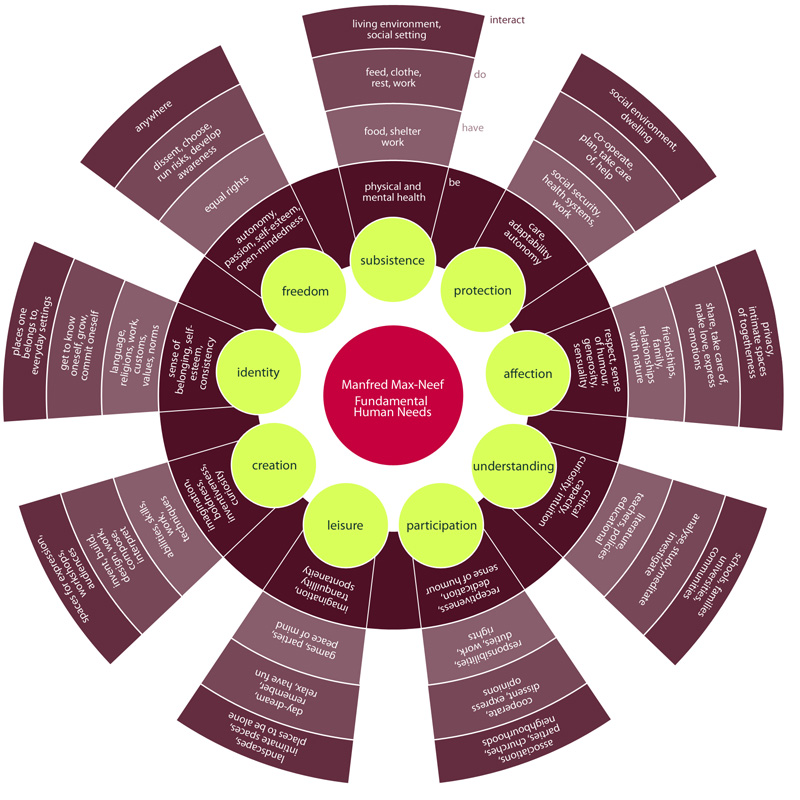
This matrix was included in the Wikipedia reference which discusses Max-Neef’s model of Universal Human Needs, which links needs with ‘satisfiers’. Again, this looks potentially really relevant to how OT’s think about maternal needs and quality of life during perinatal transitions. I can’t wait to spend more time learning about this!